Overweight and obesity specified
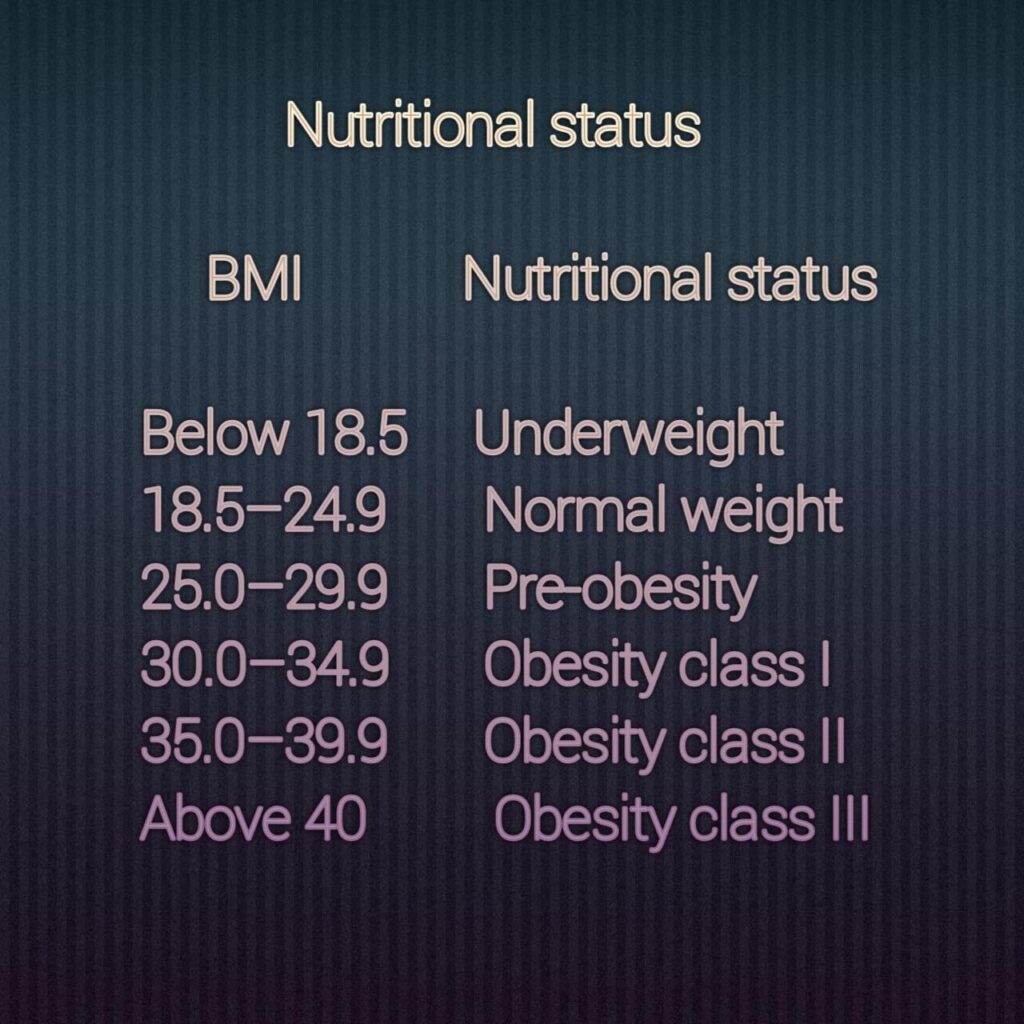
The mass index weight/height is an indirect measure of body fat and is commonly used to describe obesity. According to the Department of Health, a body fat percentage of 25-26 percent is considered overweight, while a body mass index of 29 is considered obese. Statistical research shows that obesity is becoming more common in the USA, UK., and several other nations. Nevertheless, extra intercellular fat is a distinct determinant of health risk, and the mass index does not fully describe the dispersion of fat mass. The evaluation of waist size, which corresponds with fat deposits and inferentially determines central adipose, is advised by recommendations. The Waist to hip ratio of over 0.96 for males and 0.82 for women is associated with an elevated health threat. People who are marginally or slightly overweight run the risk of being overlooked, whereas obese patients are simple to spot.
Should people who are overweight or obese be treated?
Planned weight loss reduces fatality, however, there aren’t enough research trials of weight loss therapies with enough energy to run to spot fatality disparities. Some have questioned the effectiveness of weight reduction therapies as a result of this as well as strong data demonstrating how challenging it is to maintain weight loss or gain. Nevertheless, research from randomized controlled trials, including the recently finished Diabetic Prevention Strategy, shows that lifestyle modifications and deliberate weight loss can help prevent and control chronic illnesses including type-2 diabetes and heart disease. This data supports current recommendations for weight loss in patients who are obese or overweight and have complications associated with obesity made by a group of prominent associations and governmental bodies.
Assistance and counseling in primary care
Medical practitioners need to support their patients by giving them excellent guidance on maintaining a balanced diet and increasing physical exercise. It may also be helpful to assess a patient’s willingness to modify their habit and utilize stage-specific approaches to increase helps the process. The patient should ideally have access to a multidisciplinary team that includes dietitians, kinesiotherapists, and psychiatrists.
Weight loss programs
The main components of the majority of weight loss regimens are caloric burn and physical activity levels. Although the majority of nutritionists advocate a diet high in complex carbs, low in fat intake, and modest in proteins, fashionable diets that are heavy in fat and protein and low in carbohydrates are nevertheless very common. Controlled experiments comparing these two methods are now being conducted. All patients will be able to reduce their usage of refined flour and sugar and enjoy enough protein and fiber-rich carbs to meet their basic nutritional requirements and help control hunger since many consumers are seduced by the heavy advertising of “fat-free” products, which frequently contain a large number of simple carbohydrates.

Additional measures to enhance the care of overweight and obese adults
Ample data support the claim that exercise improves cardiovascular fitness without causing significant weight reduction. Cognitive behavioral therapies that promote weight loss include ego. The best method for reducing weight and keeping it off is to use “Lifestyle” methods that include restricted calorie food, more exercise, and behavioral therapies.
Even though most people will benefit from these fundamental approaches, patients with weight-related chronic health conditions can sometimes require a few modifications. For instance, some patients may be reluctant or fearful of workouts, but even the physically weakest patients can safely engage in and gain from exercise and diet with the right assistance. Non-weight bearing workouts, like water aerobics, may be helpful for patients with chronic degenerative joint or other painful chronic diseases. Patients with osteoarthritis must maintain acceptable levels of calcium absorption when decreasing calories, but patients with diabetes may need to decrease their medication consumption to prevent clinical hypoglycemia.

Overweight and obesity are associated with emotional and social issues
Patients who are obese may put off getting medical treatment out of humiliation or fear of being mocked. Vast examination robes and reclining chairs, as well as other straightforward steps like weighing patients in a private space, may be helpful. Physicians should convey unmistakable messages to patients about the dangers of obesity, but they should avoid “blaming the victim” and handle questions about weight management in a way that doesn’t demoralize them. Stop triggering unrealistic goals to reach your “desirable” weight. Major health benefits, including better glycemic management, blood pressure control, and reductions in other heart disease risks, can be obtained by slow, significant weight loss, which is more practical. and also, broader effects including boosted vitality, adequate sleep, and higher flexibility. Family engagement may be beneficial in slowing the growth of childhood obesity, but it is unclear how this strategy would affect adults. Obese adults claim that family opposition to lifestyle changes can be a deterrent to losing weight. Obstacles that can impede even the most driven patient should be dealt with by professionals.
There are occasions when measures are taken to combat the rise in overweight and obesity, such as taxation on specific foods and drinks, restrictions on advertising, a restriction on chocolate drinks in schools, or mandated physical activity for obese workers, which raise concerns about what is morally acceptable. These projects have clear ethical benefits, including enhancing individual and public health, facilitating informed decision-making, and lowering society expenses. We focus on potential ethical arguments against such an effort, even if we believe that these favorable arguments for making significant efforts to prevent overweight are unquestionable.









Comments 1